What is Shared Decision Making?
Shared decision making is the term used to describe the joint process in which a healthcare professional works together with a person to reach a decision about their care and treatment options.
It ensures that tests and treatments are jointly chosen based on evidence and what matters to the person, their individual goals, preferences, beliefs and values.
The process of shared decision making makes sure the person understands the risks, benefits and possible consequences of different options through discussion and information sharing.
A shared decision making conversation brings together:
- The healthcare professionals expertise, such as treatment options, evidence, risks and benefits.
- What matters to the person, their preferences, personal circumstances, goals, values and beliefs.
Why is it important?
Shared decision making puts people in control of their care by considering what matters to them. It has been proven to improve compliance with treatments and reduce harm from medicines.
Shared decision making is high up on the NHS’ agenda. It is one of the six approaches of the NHSE universal personalised care model. It is also an essential part of the Professional Codes of Conduct and Standards, the General Medical Council, 2020, the Nursing and Midwifery Council, 2018 and Health and Care Professions Council, 2018 and NICE guidance.
Research tells us that people want to be more involved than they currently are in making decisions about their own health and health care. Both individuals and clinicians tend to consistently over-estimate the benefits of treatments and under-estimate the harms.
Read more about the benefits of shared decision making
Prepared Public – It’s Ok to Ask
One of the four key areas to shared decision-making is a prepared public. The Patient Information Forum (PIF) and the Patients Association worked with NHS Nottingham and Nottinghamshire Integrated Care Board (ICB) to look at ways of making it easier for patients to take part in shared decision-making.
Together we delivered a co-production programme with My Life Choices – a co-production group of people with lived experience NHS Nottingham and Nottinghamshire personalised care team. Removing Barriers to Shared Decision-Making provides the key learnings and outcomes from the project.
The outcome of the project is that the system adopted the recommendations and use It’s ok to ask to prepare the public for a shared decision-making conversation.
Please find resources below that you can use in your healthcare settings to support shared-decision making with your patients.
Resources you can use
It’s OK to ask poster
Download the ‘It’s OK to ask’ poster and use it in waiting rooms and public spaces.
It’s OK to ask webpage
The It’s OK to ask web page is a great place to your direct patients to for more information.
Webpage – It’s ok to ask – NHS Nottingham and Nottinghamshire ICB
It’s OK to ask film
This film explains the importance of it’s OK to ask.
Youtube – It’s ok to Ask (youtube.com)
About Me form
Encourage your patients to fill in an ‘about me’ form prior to any appointments. You can find information below on how to fill in the form, why it is important and useful resources you can share with your patients.
It’s OK to ask appointment letter insert
Use our letter insert in appointment letters to encourage your patients to think about any questions they may have in advance.
Its ok to ask branding for websites
Our it’s Ok to Ask banners can be downloaded and used in your own resources and websites.
Shared Decision Making postcard prompt for staff
This shared decision postcard can be printed and used as a prompt in your appointments with patients.
Shared decision-making implementation checklist
Download our implementation checklist. The checklist is a practical tool to help you start, or continue, conversations to understand where you are in your organisation, team or service on shared decision-making and support local improvements.
Decision support tools
Decision support tools (also called ‘patient decision aids’) encourage personalised care by supporting the process of shared decision making. NHS England has partnered with patients, risk communication experts and clinical leaders to co-produce a series of DSTs. These tools are designed to be used within or alongside clinical consultations and for patients to keep for reference and reflection. You may choose to use them before, in, or between consultations.
NHS England shared decision making summary guide
This summary guide is aimed at people leading local implementation of shared decision
making (SDM). It enables:
- increased understanding of what good SDM looks like and how it ensures that we commission and provide systems and services that informed individuals want
- commissioning of local SDM initiatives and embedding them in care pathways
- providers to have better conversations with people using services, thereby supporting them to make more informed choices based on their personal values and preferences and what is known of the risks, benefits and consequences of the options available to them.
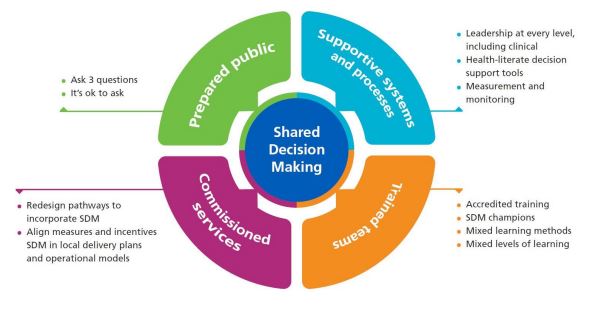
The summary guide provides an implementation framework stating that 4 key areas need to be in place to embed SDM:
Me and my medicines
‘Me and My Medicines’ is a campaign led by patients and supported by clinical staff to help people raise concerns and use their medicines better. This will help everyone benefit from more effective and safer care. Patients, families and carers are encouraged to ask questions about their medicines so that they can be helped to get the most benefit. Find out more information on the ‘Me and my medicines’ website.
Training
You can find lots of helpful tools and training to support you and your teams to learn more about the importance of shared decision making.
Your learning options (personalisedcareinstitute.org.uk)
An online learning resource to embed shared decision-making
Virtual Patient Avatars (personalisedcareinstitute.org.uk)
FAQs for health professionals
Why should I prioritise Shared Decision Making, I only have very short amount of time to see patients?
Whilst it may take a little longer to have initial conversation in a more personalised way, shared decision making ensures that individuals are supported to make decisions that are right for them, which in the longer term means fewer follow up queries and overall it makes the whole patient pathway more efficient.
Why do we need this, I am approachable?
Our patients do not always feel empowered to ask as there is a knowledge and power dynamic. Shared decision making conversations can support people to be able to feel more confident to make choices that are right for them. Consistent feedback is that people do not always feel viewed as a partner in their healthcare, more as a passive recipient.
How is this relevant to my practice?
Most of our interactions involve treatment of some kind, and consenting to treatment requires first understanding what matters most to a patient, as outlined in the GMC guidance. Shared decision making supports people to be able to tell you what matters to them to guide your professional advice and options in an individualised way to get to the right outcome.
Will a Shared Decision Making approach take longer?
Encouraging people to come with questions and write down what matters to them before they come to a consultation will help to make things more efficient as the groundwork of thinking about what matters to them has been completed.
Will this mean that people can demand certain treatments?
The law is clear that whilst patients have the right to ask questions and make decisions about what care meets their needs based on the benefits, risks, alternative and ‘do nothing’ options, it is up to the professional to describe what options would be suitable treatments.