Difficulty breathing and wheeze

- It is extremely scary if your child has any sort of breathing difficulty. Use your instincts; if your child appears well and their breathing difficultly improves after a short period, there is normally no need to worry
- Wheeze is extremely common in young children and is most often triggered by a viral infection. Most pre-school children with wheeze do not have asthma
- Children under 2 years of age with breathing difficulty may have bronchiolitis. This is an extremely common condition that usually starts as a runny nose and cough but their breathing may get worse over the next 2-3 days
- If your child is struggling to breath, they need to be urgently seen by a medical practitioner and are likely to need treatment. If your child has croup (hoarse voice, barking cough, noisy breathing), they will also need to be seen by a medical practitioner
- Most chest infections are caused by viruses and do not usually need treatment with antibiotics
- If your child has a salbutamol (blue inhaler) then follow the action plan
Operation Ouch – Breathing
When should you worry?
If your child has any of the following:
- Is going blue around the lips
- Has pauses in their breathing (apnoeas) or has an irregular breathing pattern or starts grunting
- A harsh breath noise as they breathe in (stridor) present all of the time (even when they are not upset)
- Seems dehydrated (sunken eyes, drowsy or not had a wee or wet nappy for 12 hours)
- Too breathless to talk/eat or drink
- Becomes pale, mottled and feels abnormally cold to touch
- Becomes extremely agitated (crying inconsolably despite distraction), confused or very lethargic (difficult to wake)
- Develops a rash that does not disappear with pressure (the ‘Glass Test’)
- Is under 3 months of age with a temperature of 38°C / 100.4°F or above (unless fever in the 48 hours following vaccinations and no other red or amber features)
- Is between 3-6 months of age with a temperature over 39°C
You need urgent help
Go to the nearest Hospital Emergency (A&E) Department or phone 999
If your child has any of the following:
- Has laboured/rapid breathing or they are working hard to breathe – drawing in of the muscles below their lower ribs, at their neck or between their ribs (recession)
- A harsh breath noise as they breathe in (stridor) present only when they are upset
- Seems dehydrated (sunken eyes, drowsy or not had a wee or wet nappy for eight hours)
- Is becoming drowsy (excessively sleepy) or irritable (unable to settle them with toys, TV, food or picking up) – especially if they remain drowsy or irritable despite their fever coming down
- Has extreme shivering or complains of muscle pain
- Is 3-6 months of age with a temperature of 39°C / 102.2°F or above (but fever is common in babies up to 2 days after they receive vaccinations)
- Continues to have a fever of 38.0°C or above for more than 5 days
- Is getting worse or if you are worried
You need to contact a doctor or nurse today
Please ring your GP surgery or call NHS 111 – dial 111
We recognise that during the current COVID-19 crisis, at peak times, access to a health care professional may be delayed. If symptoms persist for 4 hours or more and you have not been able to speak to either a member of staff from your GP practice or to NHS 111 staff, then consider taking them to your nearest Emergency Department
If none of the above features are present
Make sure that your child stays well hydrated by offering them lots of fluids. Closely monitor them for any signs of deterioration by looking out for any red or amber features
Additional advice is also available for families for help cope with crying in otherwise well babies.
Self care
Continue providing your child’s care at home. If you are still concerned about your child, call NHS 111 – dial 111
What should you do?
- If your child is interacting with you normally and is able to drink as normal, you can watch them closely at home. If your child is not feeding as well as normal, you should offer smaller feeds but more frequently
- If they become more breathless or are struggling to drink, they will need to be seen urgently by a medical practitioner. Call your GP surgery or NHS 111
- If your child has a fever, their breathing may become more rapid. You should try to lower their temperature using paracetamol (calpol)
How long will your child’s symptoms last?
- Although your child’s cough is likely to last for 2 to 3 weeks, they should not be breathless or wheezy for more than 3 or 4 days
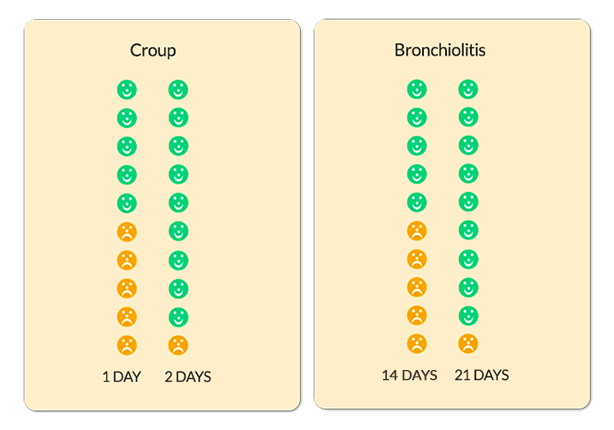
- The charts below show how long croup or bronchiolitis last in children. The faces represent 10 children who have croup or bronchiolitis. Green faces are those children who have recovered within that time period
Where should you seek help?
- If it is non-urgent, speak to your local pharmacist or health visitor.
- If your child has any of the above features, urgently see your GP. For an urgent out-of-hours GP appointment, call NHS 111.
- You should only call 999 or go your nearest A&E department in critical or life threatening situations.